Initial evaluation and management of small and moderate burns is a routine part of general plastic surgery practice. An ability to accurately evaluate and provide proper initial care for these injuries is essential.
Outcomes for patients with burns have improved dramatically over the past 20 years, but burns still cause substantial morbidity and mortality.1 Proper evaluation and management, coupled with appropriate early specialty referral, greatly help in minimizing suffering and optimizing results.2
For excellent patient education resources, visit eMedicine's Burns Center. Also, see eMedicine's patient education article Thermal (Heat or Fire) Burns.
Evaluation of the Burn Patient
Before management of the burn wound can begin, properly and completely evaluate the burn patient. Often this is a brief effort, particularly in patients with small, uncomplicated wounds. In those with larger burns, evaluation of the wound often is of secondary importance. As described by the American College of Surgeons Committee on Trauma, evaluation of the burn patient is organized into a primary and secondary survey.
Primary survey
Burn patients should be systematically evaluated using the methodology of the American College of Surgeons Advanced Trauma Life Support Course. This evaluation is described by the primary survey, with its emphasis on support of the airway, gas exchange, and circulatory stability. First evaluate the airway; this is an area of particular importance in burn patients. Early recognition of impending airway compromise, followed by prompt intubation, can be life saving. Obtain appropriate vascular access and place monitoring devices, then complete a systematic trauma survey, including indicated radiographs and laboratory studies.
Secondary survey
Burn patients should then undergo a burn-specific secondary survey, which should include determination of the mechanism of injury, evaluation for the presence or absence of inhalation injury and carbon monoxide intoxication, examination for corneal burns, consideration of the possibility of abuse, and a detailed assessment of the burn wound. (Click here to complete a Medscape CME activity on carbon monoxide screening.)
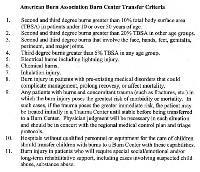
A detailed history must be elicited upon first evaluation and transmitted with the patient to the next level of care. Inhalation injury is diagnosed by a history of a closed-space exposure and soot in the nares and mouth. Carbon monoxide intoxication is suspected in those injured in structural fires, particularly if they are obtunded; carboxyhemoglobin levels can be misleading in those ventilated with oxygen. Those with facial burns should undergo a careful examination of the cornea prior to the development of lid swelling that can compromise examination. After evaluation of the burn wound, begin fluid resuscitation and make decisions concerning outpatient or inpatient management or transfer to a burn center (see Image 1).
Evaluation of the Burn Wound
After the patient has been fully evaluated and stable hemodynamics and gas exchange ensured, evaluate the burn wound in detail. Evaluate burn wounds initially for extent, depth, and circumferential components. Decisions regarding type of monitoring, wound care, hospitalization, or transfer are made based on this information.
Extent of burn
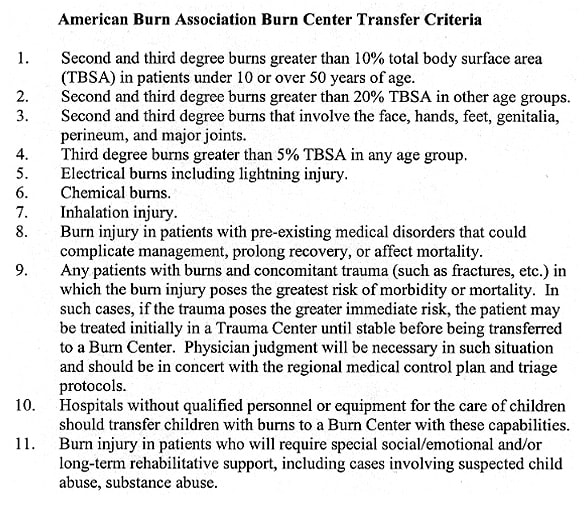
An accurate estimate of burn size is important for treatment and transfer decisions. Burn size or extent can be estimated in numerous ways. Perhaps most accurate is the age-specific chart based on the Lund-Browder diagram that compensates for the changes in body proportions with growth (see Image 2). A burn is drawn on a cartoon figure and an associated age-specific table is used to calculate the body surface area involved.
An alternative in adults is the Rule of Nines. This is less accurate in children because their body proportions are different than those of adults. For areas of irregular or nonconfluent area burns, the palmar surface of the patient's hand can be used. For a wide age range, the area of the palm without the fingers represents 0.5% of the body surface.
Burn depth
Burns are routinely underestimated in depth on initial examination. Devitalized tissue may appear viable for some time after injury, and often, some degree of progressive microvascular thrombosis around the periphery of wounds is seen. Consequently, the wound appearance changes over the days following injury. Serial examination of burn wounds can be very useful.
Burn depth is classified as first, second, third, or fourth degree.
- First-degree burns usually are red, dry, and painful. Burns initially termed first degree often are actually superficial second degree, sloughing the next day.
- Second-degree burns often are red, wet, and very painful. Their depth, ability to heal, and propensity to form hypertrophic scars varies enormously (see Image 3).
- Third-degree burns generally are leathery in consistency, dry, insensate, and waxy. These wounds will not heal, except by contraction and limited epithelial migration with resulting hypertrophic and unstable cover (see Image 4). Burn blisters (see Image 5) can overlie both second-degree and third-degree burns. The management of burn blisters remains controversial, yet intact blisters help greatly with pain control. Debride blisters if infection occurs.
- Fourth-degree burns involve underlying subcutaneous tissue, tendon, or bone. Accurately determining burn depth on early examination is usually very difficult, even for an experienced examiner. As a general rule, burn depth is underestimated on initial examination.
Please also see eMedicine article Burns, Thermal for further information on the depth of burn injury and its effect on the skin.
Note circumferential, or near circumferential, burn wounds because they may cause progressive extremity ischemia or interfere with ventilation as burn wound swelling increases. In such situations, timely escharotomy is essential. Perform extremity escharotomies as soon as peripheral perfusion is threatened. Do not wait until the extremity is overtly ischemic. Perform torso escharotomies as soon as ventilation appears compromised.
Burn Wound Infection
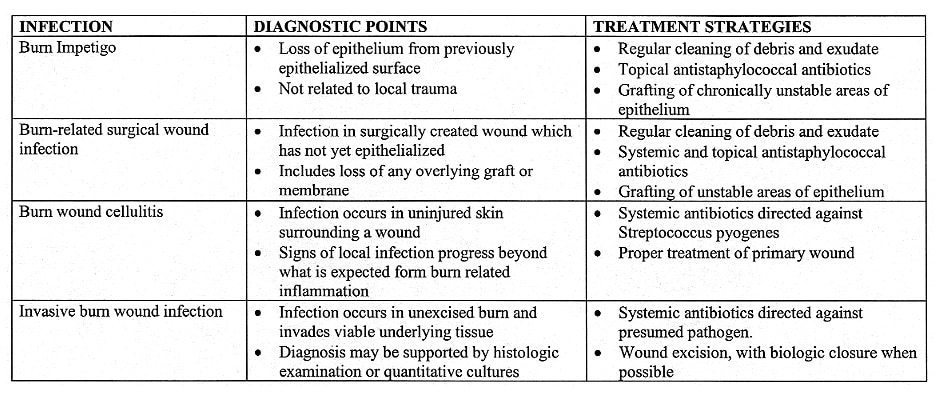
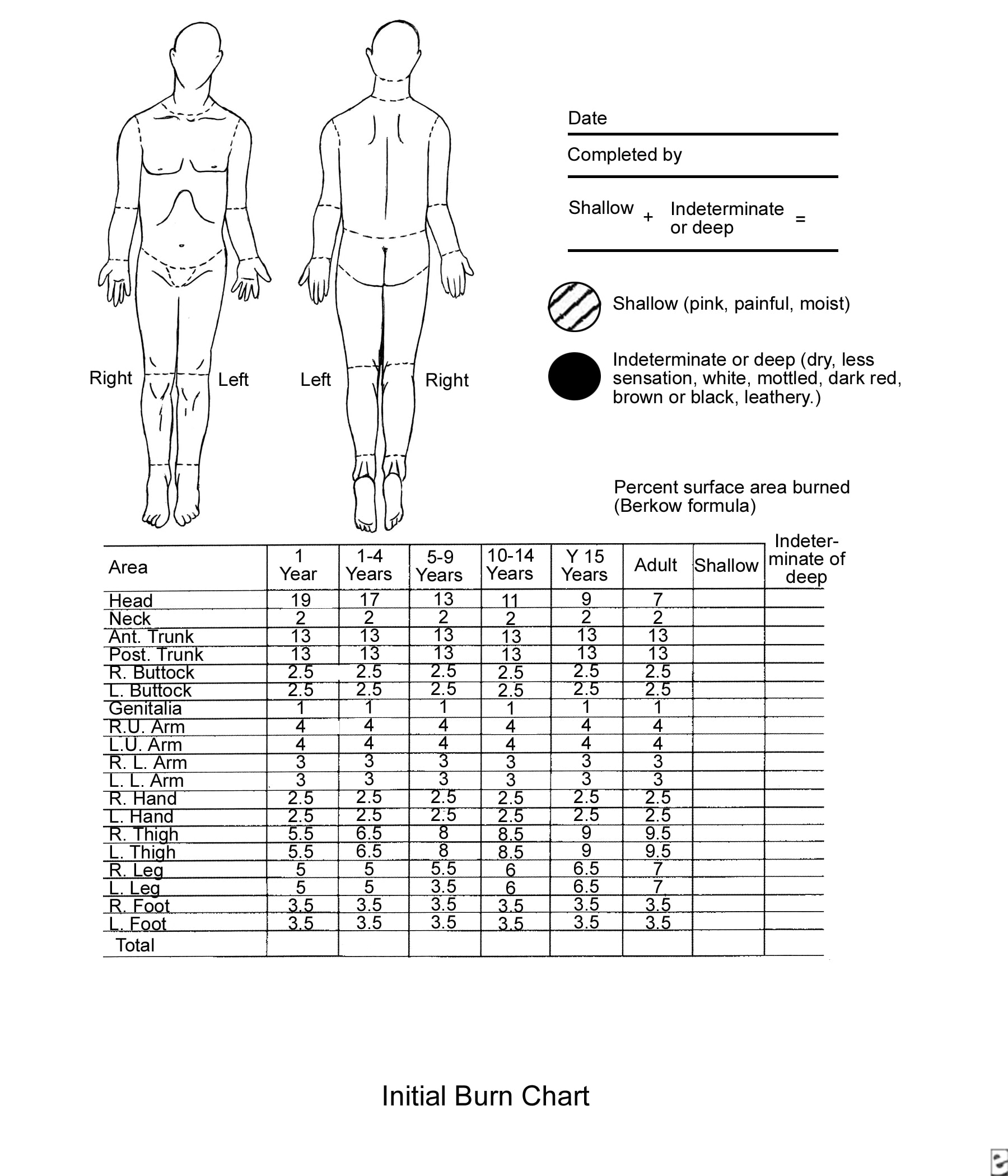
An ability to make the diagnosis of burn wound infection is important. A clinically focused set of burn wound infection definitions recently has been published (see Image 6). Two of these, burn wound cellulitis and invasive burn wound infection, are seen with some regularity by clinicians outside a burn center environment.
Burn wound cellulitis (see Image 7) usually manifests as progressive erythema, swelling, and pain in the uninjured skin around a wound. Usually, this is seen in the first few days after burning and typically is caused by Streptococcus pyogenes. Infection can progress rapidly but is generally sensitive to penicillin. Excision of associated deep eschar can be essential to the successful treatment of cellulitis. Elevation to reduce edema is an important adjunct.
Invasive burn wound infection (see Image 8) is a rapid proliferation of bacteria in burn eschar that proceeds to invade underlying viable tissues. A change in color, new drainage, and, occasionally, a foul or sickly sweet odor are clinical findings. Pseudomonas and other gram-negative species are common causes. This infection can be life-threatening and usually requires combined treatment with surgery and antibiotics.
Fever and systemic toxicity commonly accompany both infections. Inspect burn wounds frequently to identify infection early. This is an important consideration in outpatient burn care. Someone must inspect the wounds managed in the outpatient environment to promptly detect infections. Errors in initial depth assessment are routine. Infections occur and must be treated in a timely way. A wound-monitoring plan is an essential part of burn care.
Burn Wound Management
Most burns are small; patients with small burns are appropriately managed as outpatients if their burns do not involve critical areas such as the face, hands, genitals, or feet. The outpatient setting is the primary focus of this section. Outpatient burn management can be taxing and, when poorly performed, can cause unnecessary suffering and compromise long-term results. In some situations, coordinating outpatient management with the burn unit's team of doctors, nurses, and therapists is helpful, as their expertise may facilitate attaining optimal outpatient results; however, most small burns are well managed by community based providers with burn center consultation as needed.
Selection for outpatient care
Several factors are relevant to a decision regarding the location of burn care. The patient's airway must not be potentially compromised. The wound must be small enough so that fluid resuscitation is unnecessary (this generally precludes outpatient care of burns over 10-15% of body surface). Patient must be able to take in adequate fluid orally. Typically, serious burns of the face, ears, hands, genitals, or feet should be initially managed on an inpatient basis.
The patient and his or her family must be able to support an outpatient care plan. A child managed as an outpatient must have an adult caregiver available. A family member or visiting nurse must be available who can perform the necessary wound cleansing, inspection, and dressing applications, as most patients cannot do this themselves. Family must have adequate transportation to return for clinic visits and unexpected emergency visits. If abuse is suspected, outpatient management is contraindicated. Finally, if, on initial examination, surgery is clearly needed for a full-thickness wound area, the patient should be admitted for surgery promptly. Despite all of these qualifications, most patients with smaller burns can be successfully managed as outpatients.
Outpatient wound care strategies
Components of outpatient burn care include the following:
- Patient and family education
- Wound cleansing
- Choice of topical or membrane dressing
- Pain control
- Early return instructions
- Follow-up clinic visits
- Long-term follow-up care
Wound cleansing and dressing techniques must be taught to the person who changes the dressings. Documenting this teaching is ideal.
Which of many medications or membranes to place on burn wounds remains unclear, but certain basic principles apply to all situations. Gently clean the wound of debris and exudate on a regular basis. This usually requires daily removal of accumulated exudate and topical medications. Small superficial burns managed in this setting present a low risk of infection, thus a clean rather than sterile technique is reasonable. Patients may clean the burn with lukewarm tap water and mild soap.
Soaking dressings in lukewarm tap water may decrease the pain associated with their removal. Gently cleanse the wound with a gauze or clean washcloth, inspect for signs of infection, pat dry with a clean towel, and re-dress the patient. To manage infections promptly, it is important to teach the patient and family to return promptly if they notice erythema, swelling, increased tenderness, odor, or drainage. Frequency of wound cleansing and dressing change is debated, but most small burns are managed adequately with daily cleansing and dressing.
Wound dressing, whether one is using topical medication or a wound membrane, should provide 4 benefits: (1) prevention of wound desiccation, (2) control of pain, (3) reduction of wound colonization and infection, and (4) prevention of added trauma to the wound. Most topicals in outpatient use have a viscous carrier that prevents wound desiccation and a broader antibacterial spectrum that reduces wound colonization. Addition of a gauze wrap minimizes soiling of both clothing and unburned skin and protects the wound from the external environment. A large number of excellent agents are available.
Superficial facial burns are commonly treated with a clear, viscous antibacterial ointment. Wounds around the eyes can be treated with heavy topical ophthalmic antibiotic ointments. For more information, see eMedicine article Burns, Ocular. Treat deep burns of the external ear with mafenide acetate, as it penetrates the eschar and prevents purulent infection of the cartilage. Appropriate wound care strategies address these principles.
Control of pain in the outpatient setting can be difficult, and if pain and anxiety cannot be adequately managed at home, then hospitalization is appropriate. In most patients, an oral narcotic medication administered 30-60 minutes prior to a planned dressing change provides adequate pain control. As most dressings are occlusive, pain control between dressing changes tends to be managed adequately without narcotics in most patients.
Elaborate specific conditions mandating an early return. Particularly important are (1) pain and anxiety associated with wound care to the degree that wound care is compromised, (2) signs of infection, or (3) a wound that appears deeper than appreciated at initial examination. Review wound care instructions with caregivers.
Inpatient management
The plan of management of patients with large burns that require inpatient care usually is determined by the physiology of burn injury. Management strategies for these patients are beyond the scope of this article but generally require a coordinated approach that involves a specialized team. Hospitalization is divided into 4 general phases: (1) initial evaluation and resuscitation, (2) initial wound excision and biologic closure, (3) definitive wound closure, and (4) rehabilitation and reconstruction.
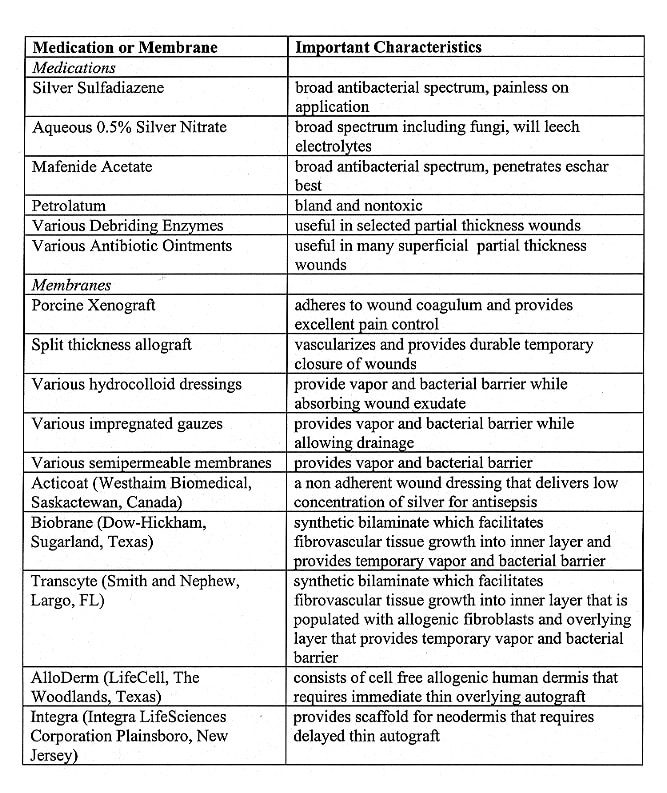
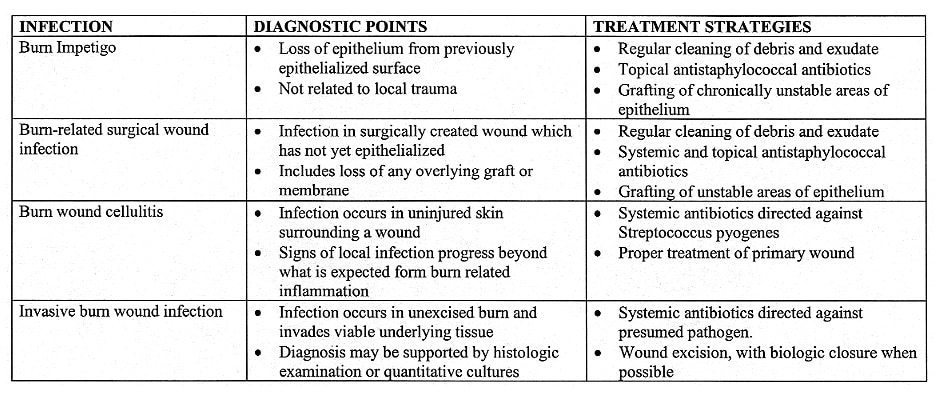
Medications and Membranes
The choice of which medication or membrane to place on a wound is a neverending source of discussion and argument. Fortunately, most medications and membranes perform well if physicians carefully monitor wounds, keep them clean, prevent desiccation, and properly manage secondary infection.
A wide range of topical medications is available, including simple petrolatum, various antibiotic-containing ointments and aqueous solutions, and debriding enzymes. Some of the available topical medications and their characteristics are listed in Image 9. All of them can be effectively employed when properly used by experienced providers in a program of burn care that includes wound evaluation, regular cleansing, and monitoring.
Wound membranes are different from medications and dressings in that they provide transient physiologic wound closure. This implies a degree of protection from mechanical trauma, vapor transmission characteristics similar to skin, and a physical barrier to bacteria. These membranes facilitate a moist wound environment with low bacterial density. They are commonly placed on clean superficial wounds while awaiting epithelialization. These membranes are mostly occlusive; therefore, they must be used with caution if wounds are not clearly clean and superficial. If an occlusive membrane is placed over devitalized tissue, submembrane purulence can occur with subsequent local and systemic sepsis. A large number of these membranes are available (see Image 9).
Wounds in Special Areas
Face, ears, hands, genitals, and feet have functional and cosmetic significance that far exceeds their size and physiologic importance. The surface area involved is such that burn sepsis from these sources rarely is life-threatening, and a studied approach to these wounds usually is possible.
Face
Especially in adolescents and adults, the deep sweat and sebaceous glands of the central face make it likely that most second-degree burns will heal well with adequate topical wound care. Many reasonable management options are available, including topical silver sulfadiazine or bland antibiotic ointments. Burns around the eyes can be dressed with topical ophthalmic antibiotic ointments. If grafting is a possibility, reserve thick donor skin with optimal color match for facial resurfacing. Often, the "blush" areas, such as the upper back and shoulders, make good facial donor sites.
The most important point of early management of deeply burned ears is prevention of auricular chondritis. This is a serious complication in which the cartilage becomes infected and quickly liquefies. Twice daily cleansing and application of topical mafenide acetate, which penetrates the eschar, can minimize the condition. Subsequent management of the ear is based on depth of injury.
Deep corneal burns are obvious on physical examination. The cornea has a clouded appearance. More subtle injuries can be detected only with topical fluorescein application. After facial edema resolves, lid retraction may occur with variable degrees of exposure of the globe or ectropion. When this is relatively mild, no intervention is required beyond ocular lubricants. Should keratitis occur, early lid release is advised.
Hand burns
Hand burns assume a high priority from the onset of care. During the first 24-48 hours, adequate blood flow must be ensured. Regularly monitor consistency, temperature, and the presence of pulsatile flow detectable by Doppler in the digital pulp. If blood flow is questionable, perform escharotomy or fasciotomy.
Splint hands in a position of function: the metatarsophalangeal joints at 70-90 º, interphalangeal joints in extension, first web space open, and wrist at 20 º of extension. Elevate hands to minimize edema and have the patient perform range-of-motion exercises with a therapist twice daily. Deep dermal and full-thickness burns should undergo early excision and sheet autograft closure. Perform hand therapy throughout the healing period, halting only in the few days immediately after grafting. If this is not done, suboptimal long-term function results (see Image 10).
Conclusions
After making a careful initial evaluation, refer patients with complex, deeper, or larger wounds for specialty care. In others, application of basic principles of management combined with regular monitoring constitutes adequate therapy and leads to routinely good results.
Multimedia
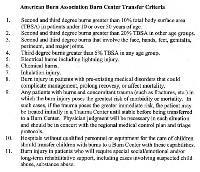 | Media file 1: American Burn Association has developed a set of criteria for burn center transfer. These have been adopted by most emergency medical services. |
American Burn Association has developed a set of criteria for burn center transfer. These have been adopted by most emergency medical services.
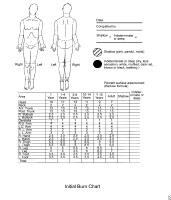 | Media file 2: Burn size is best estimated using a chart that corrects for changes in body proportion with aging. |
Burn size is best estimated using a chart that corrects for changes in body proportion with aging.
 | Media file 3: Second-degree burns often are red, wet, and very painful. Their depth, ability to heal, and tendency to result in hypertrophic scar formation vary enormously. |

Second-degree burns often are red, wet, and very painful. Their depth, ability to heal, and tendency to result in hypertrophic scar formation vary enormously.
 | Media file 4: Third-degree burns usually are leathery in consistency, dry, and insensate. These wounds will not heal. |

Third-degree burns usually are leathery in consistency, dry, and insensate. These wounds will not heal.
 | Media file 5: Management of burn blisters is controversial. Burn blisters occasionally obscure the presence of full-thickness wounds. |

Management of burn blisters is controversial. Burn blisters occasionally obscure the presence of full-thickness wounds.
 | Media file 6: This clinically focused definition set describes burn wound infections. |
This clinically focused definition set describes burn wound infections.
 | Media file 7: Burn wound cellulitis presents with increasing erythema, swelling, and pain in uninjured skin around the periphery of a wound. |

Burn wound cellulitis presents with increasing erythema, swelling, and pain in uninjured skin around the periphery of a wound.
 | Media file 8: Invasive burn wound infection implies that bacteria or fungi are proliferating in eschar and invading underlying viable tissues. These wounds display a change in color, new drainage, and often a foul odor. These infections are life-threatening. |

Invasive burn wound infection implies that bacteria or fungi are proliferating in eschar and invading underlying viable tissues. These wounds display a change in color, new drainage, and often a foul odor. These infections are life-threatening.
 | Media file 9: Numerous topical medications and membranes have a place in burn care. |
Numerous topical medications and membranes have a place in burn care.
 | Media file 10: If hand positioning and therapy are ignored while overlying burns heal, poor long-term function may result. |

If hand positioning and therapy are ignored while overlying burns heal, poor long-term function may result.
 | Media file 11: |
 | Media file 12: |